Enhanced Recovery After Surgery (ERAS) in Urologic Oncology
Enhanced Recovery After Surgery (ERAS) in urologic oncology is transforming how patients heal after major procedures. By combining evidence-based protocols with multidisciplinary collaboration, ERAS improves outcomes while reducing hospital stays and complications.
ERAS protocols are now considered a cornerstone of modern perioperative care. Particularly in the realm of urologic cancer surgeries—such as radical prostatectomy, cystectomy, and nephrectomy—these protocols are reshaping the patient experience. Enhanced Recovery After Surgery in urologic oncology not only promotes faster recovery but also enhances long-term well-being.
What Is ERAS and Why Does It Matter?
ERAS is a patient-centered approach that optimizes recovery through a series of standardized yet flexible interventions before, during, and after surgery. Unlike traditional care models, ERAS aims to:
-
Minimize surgical stress response
-
Promote early mobilization
-
Encourage prompt return to normal nutrition
-
Reduce opioid dependence
In urologic oncology, where procedures are often extensive and physically taxing, ERAS protocols help patients regain strength sooner and resume normal life with fewer setbacks.
How ERAS Elevates Outcomes in Urologic Oncology
The implementation of ERAS in urologic oncology is supported by robust clinical data. Studies consistently demonstrate:
-
Shorter hospital stays: Many patients are discharged 1–3 days earlier than with conventional recovery.
-
Lower complication rates: Reduced incidence of ileus, infections, and thromboembolic events.
-
Better pain management: Multimodal analgesia reduces opioid use and related side effects.
-
Higher patient satisfaction: Patients feel more informed, empowered, and in control of their healing process.
These results are especially important in complex surgeries like robot-assisted radical cystectomy, where traditional recovery can be prolonged and painful.
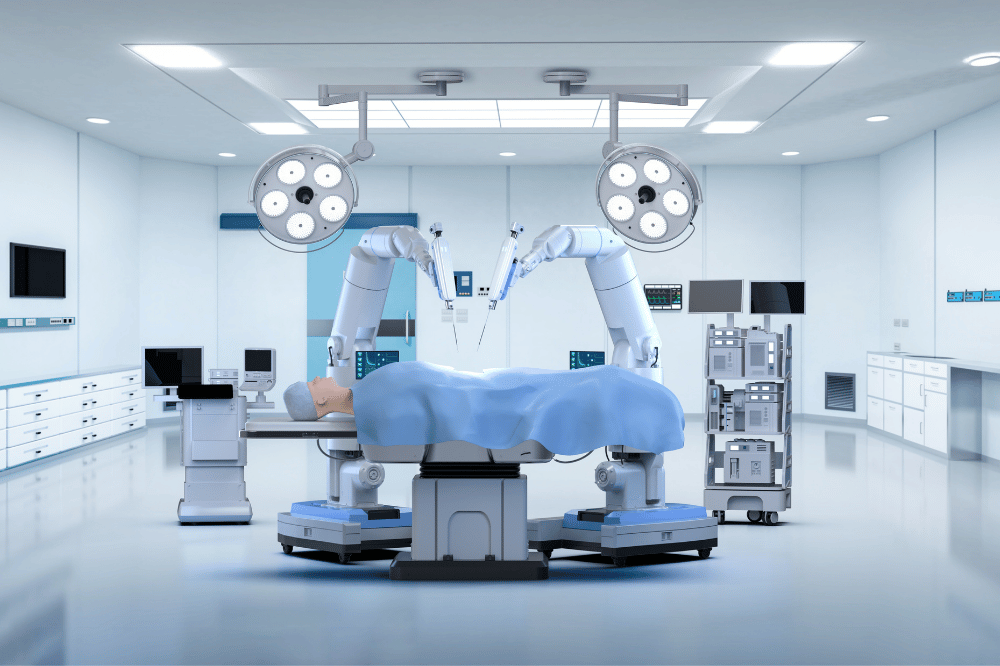
The Synergy Between Robotic Surgery and ERAS
Robotic-assisted surgeries—already known for minimizing tissue trauma and blood loss—complement ERAS principles beautifully. For example:
-
Precision and less invasiveness reduce postoperative inflammation and pain.
-
Faster ambulation is easier with smaller incisions.
-
Fewer drains and catheters align with early mobilization goals.
When robotic techniques are combined with ERAS protocols, the recovery curve is even steeper—benefitting both patients and healthcare systems.
Key Components of ERAS in Urologic Cancer Surgery
While protocols may vary by institution, typical ERAS elements in urologic oncology include:
Preoperative Phase
-
Nutritional screening and optimization
-
Smoking and alcohol cessation
-
Detailed patient education and expectation management
-
Carbohydrate-rich drinks up to 2 hours before surgery
Intraoperative Phase
-
Minimally invasive surgical approach (robotic where applicable)
-
Short-acting anesthetics and fluid optimization
-
Normothermia maintenance
-
Proactive nausea control
Postoperative Phase
-
Early removal of catheters and drains
-
Immediate return to oral nutrition
-
Early and frequent ambulation
-
Multimodal pain control avoiding heavy opioids
Clinical Evidence Supporting ERAS in Urologic Oncology
A 2021 meta-analysis found that ERAS pathways in radical cystectomy led to:
-
25% reduction in length of stay
-
32% decrease in overall complications
-
Significant improvement in 30-day readmission rates
Similar benefits were observed in robotic partial nephrectomy and laparoscopic prostatectomy cases. These studies underline how ERAS is not just theory—it’s a clinically validated tool.
Common Questions About ERAS in Urologic Cancer Surgery
Is ERAS safe for elderly or high-risk patients?
Yes. In fact, ERAS protocols can be especially beneficial for frail individuals by reducing stress and accelerating mobilization.
Does ERAS increase surgical costs?
While some resources are allocated upfront (e.g., nutritional counseling), overall costs drop thanks to reduced complications and shorter hospitalizations.
Can ERAS be personalized?
Absolutely. While the protocols are standardized, each plan is tailored to the patient’s condition, surgery type, and preferences.
Promoting a Patient-First Culture in Oncology
As cancer care moves toward a more holistic and value-based model, ERAS in urologic oncology offers a blueprint for better outcomes. Its success lies not only in clinical algorithms but in communication, teamwork, and the shared goal of empowering patients through every stage of their cancer journey.
Hospitals and centers that embrace ERAS are sending a strong message: healing is not just about the operation—it’s about how we prepare and care for each individual, every step of the way.
Interested in how technology is reshaping surgical care? You might also enjoy reading:
These articles explore how innovation is redefining standards in modern urology.